Tumors can harbor a variety of fungi and bacteria. Understanding how cancer develops and how to treat it may depend on these microbial residents.
Other species of life can thrive in our bodies. Our guts, mouths, noses and skin support assorted networks of microorganisms that can be both great and awful for our wellbeing. However, researchers have recently discovered microbes in a completely unexpected location: tumors.
It is common to imagine cancer as nothing more than a mass of a patient’s own cells that break down and grow out of control. They are, in fact, communities of a variety of cell types, which is one reason cancers are so difficult to treat because it is hard to target them without causing harm to healthy tissue.
Yet, cancers likewise play host to an assortment of cells from other life-shapes completely – microscopic organisms and parasites. While others live inside the cancer cells themselves, some thrive in the surrounding environment of a tumor.
However, the function that these microbes play in tumors was not completely understood until relatively recently. Scientists are now beginning to determine whether these tumor-associated microorganisms are innocent bystanders caught up in the tumor or if they are partners who support cancer cells as they grow. Additionally, the answers may provide novel cancer prevention and treatment strategies.
Ravid Straussman, a cancer biologist at the Weizmann Institute of Science in Rehovot, Israel, and his team conducted a research project in 2017 and demonstrated that some bacteria that live inside human pancreatic cancers can protect the tumors by deactivating a common chemotherapy drug. They discovered that one group of bacteria, Gammaproteobacteria, could degrade gemcitabine: a treatment for a variety of cancers, including bladder, breast, and pancreatic cancers. This assisted the tumors in developing drug resistance. The bacteria were injected into colon cancer-infected mice by the team, and the cancers developed resistance to the drug as well. However, the resistance vanished when the researchers administered an antibiotic to the mice in addition to the chemotherapy drug.
In addition to these findings, a team at Tohoku University in Japan conducted a retrospective study in 2019 on patients with advanced cancer who were treated with either a chemotherapeutic drug alone or an antibiotic in addition to the chemotherapy in an effort to either treat or prevent an infection that was already present. They discovered that antibiotic-treated patients responded better to treatment. The researchers speculated that the antibiotics might have eliminated tumour-associated bacteria, which may have been interfering with the cancer treatment, despite the fact that the study did not examine the quantity of bacteria that were present in the cancer tissue of these patients.
The studies provide a tantalizing glimmer of what might be happening inside of tumors.
Now, Straussman and his team hope to expand on these studies by conducting a clinical trial with patients with pancreatic cancer who have not responded to their initial treatment. In order to determine whether the antibiotic improves patients’ outcomes, they will administer a course of the chemotherapy drug gemcitabine alongside an antibiotic that is known to be effective against Gammaproteobacteria.
However, microbes could likewise assume different parts in disease past shielding growths from drug treatment.
Over 1,500 human tumors from seven different types of cancer were examined by Straussman’s team in 2020: melanoma, bone, brain, breast, lung, ovary, and pancreas They found the growth types were all attacked by microbes, which lived inside the disease cells and a portion of the resistant cells. Different growth types had unmistakable networks of microbes.
Straussman asserts, “Each of these bacteria has adapted to the unique tumor microenvironment in which they live.” We demonstrated how smokers have more bacteria that can degrade nicotine, a metabolite of smoking, in lung cancer. Bacteria that metabolize hydroxyproline, a metabolite enriched in bone tumors, can be found in bone cancers.
In many instances, it is still not clear whether the bacteria are assisting the patient by controlling the cancer cells.
Arsenate, a carcinogen known to increase breast cancer risk, can be detoxified by bacteria found in some types of breast cancer. Mycothiol, a chemical that helps to lower levels of harmful reactive oxygen molecules that can harm DNA, can be produced by others.
However, there is increasing evidence that, in some instances, the bacteria that live in tumors may actually be making cancers worse.
“More and more papers are coming out showing how they may be part of the carcinogenesis,” says Straussman, “some bacteria in breast tumors may make it easier for cancer cells to spread to other parts of the body.” He adds, “The immune system’s ability to target and destroy cancer cells may also be being altered by the bacteria.” However, this is only the tip of the iceberg. He asserts that research into the effects that bacteria in tumors have on the progression of cancer requires a great deal more effort.
Already, there are some hints. For instance, a Chinese study from 2022 suggests that some bacteria in breast tumors may facilitate the spread of cancer cells to other parts of the body. The researchers discovered that breast tumor cells circulating in the blood of mice contained bacteria. After leaving the primary tumor, these circulating cancer cells can spread to other parts of the body, where they can grow and metastasize. On the other hand, as the tumor cells move through the bloodstream, they come into contact with stress, which causes some of them to split up.
The Chinese researchers discovered that these mobile tumor cells’ microbes appear to shield them from some of the stress they endure. They appear to accomplish this by assisting in the reorganization of the cytoskeleton—an internal support structure for cells—to increase the cell’s strength. Although the primary breast cancer continued to spread after these bacteria were removed from the tumors of the mice, it appeared that the tumors had lost their capacity for metastasis.
According to Douglas Hanahan, an oncologist at the Swiss Institute for Experimental Cancer Research in Lausanne, Switzerland, and the author of Hallmarks of Cancer: “There is growing evidence that specific microbes in the gut, the skin, and other mucosal organs, as well as in tumors, can either promote tumor growth and progression, or alternatively antagonize it,” New Perspectives However, the picture is still hazy. The landscape is very complicated, and although there are hints, it is unclear who does what.
Fusobacterium nucleatum, an oral bacterium linked to gum disease and possibly a number of other cancers, was the subject of other studies. It appears that these bacteria can travel through the bloodstream from the mouth to a colorectal cancer cell. Each bacterium has specific particles on its surface that allow it to colonize cancer cells by binding to their surface.
By hindering the immune system’s ability to eliminate cancer cells, the bacteria can accelerate the growth and spread of tumors once they are present. Fusobacterium nucleatum produces a protein that binds to a molecular control mechanism on the surfaces of human T cells and natural killer cells, which are essential components of the immune system’s defenses against tumors. This limiting restrains the cells’ capacity to obliterate disease cells. Additionally, the bacteria use a molecular arsenal to increase cancer cells’ resistance to chemotherapy.
Additionally, human breast cancer samples have been found to contain Fusobacterium nucleatum DNA. This indicates that it also affects tumors in other parts of the body. In one review, when the microbes were acquainted with mice with bosom malignant growth, it sped up the movement and spread of the illness. This was prevented by giving the mice antibiotics.
Antibiotics in cancer treatments may seem appealing, but it’s not as simple as that. According to Hanahan, because many of the microbes in our bodies are benign or even beneficial, harsh antibiotic treatment might do more harm than good.
All things being equal, scientists should attempt to unwind the full intricacy of the cancer related microbiome. Tumors can contain entire communities of microbes that support one another in unexpected ways.
The primary chemotherapeutic drug for colorectal cancer patients, 5-fluorouracil (5-FU), is one such example. It seems to stop the troublesome Fusobacterium nucleatum from growing. However, the drug is rendered inactive by certain Escherichia coli strains—common gut bacteria.
The inactive form of 5-FU no longer inhibited cancer in laboratory cell cultures, according to research led by Susan Bullman, a cancer microbiologist at the Fred Hutchinson Cancer Centre in Seattle, USA. Additionally, it no longer inhibited the growth of Fusobacterium nucleatum. Because of this, Bullman and her colleagues hypothesized that patients who did not respond to 5-FU treatment might be contaminated with bacteria that render the medication inactive. Patients’ conditions may get worse as a result of these bacteria allowing Fusobacterium nucleatum to flourish.
Additionally, you may be interested in:
How exercise can give your microbiome a lift
The microscopic organisms controlling your cerebrum
The 77-million-year-old diseases
No less than 33 unique kinds of malignant growth have now been found to have provinces of microscopic organisms related with them, on account of procedures created at the College of California, San Diego, that search for their DNA. The scientists accept the methods could likewise be utilized to foster better approaches for diagnosing disease, by searching for the DNA from particular growth related microorganisms in a patient’s blood.
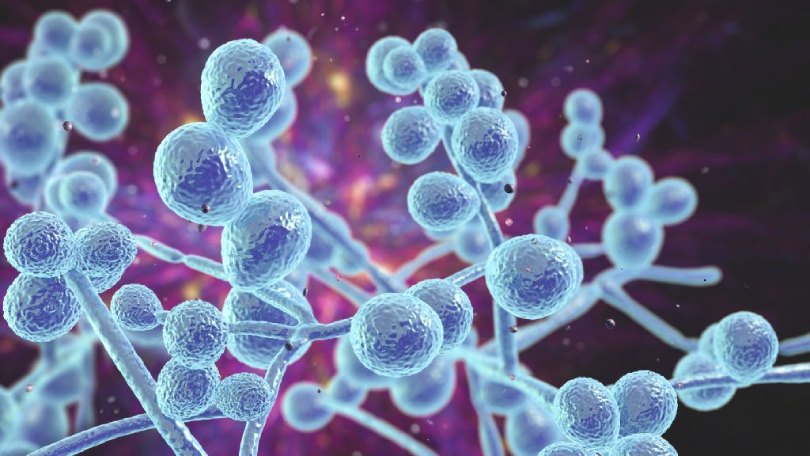
The group behind this study united with Ravid Straussman for a recent report that uncovered one more kind of microorganism – growths – living in disease. They discovered fungi in 35 distinct types of cancer, many of which contained distinct species combinations.
“We found that growths which have more microbes additionally have more organisms, and ones with less microorganisms have less parasites,” says Straussman. ” We can conjecture right now that a few growths are more prohibitive for the presence of microorganisms in them and some are more tolerant.”
Some of these fungi appear to be influencing the immune system in the tumor’s favor, just like bacteria do. One type of pancreatic cancer has been found to progress more quickly when the fungus Malassezia globosa is present. Similar growths have likewise been found in bosom disease patients who will generally have more limited by and large endurance, as per work by Straussman and his College of California, San Diego partners. Other examination has found that a few parasites present in pancreatic diseases seize portions of the resistant framework to advance cancer development.
A recent report likewise showed that stomach malignant growths wealthy in Candida parasites show expanded articulation of cancer qualities that advance irritation and that colon growths wealthy in Candida DNA are bound to be metastatic. This “may be on the grounds that expanded numbers in Candida might be related with loss of stomach epithelial boundary [the cells covering the gut],” says Iliyan Iliev, a microbiologist at Cornell College, whose group led the examination.
Despite the rapid pace of these findings, there are still many unanswered questions regarding the connection that exists between tumors and the microbes that reside within them. Is it possible that the microbes were involved in the tumor’s genesis? Or are they merely opportunistic residents who have adapted to safeguard their cancer-infected residence whenever one is discovered? Also, might this organism local area at any point be tackled to help us in our battle against malignant growths?
Targeting tumor microbes may become as crucial in the coming years as pursuing cancer cells themselves, resulting in earlier diagnoses and even novel treatments. However, that work has only begun.